Definition
Encephalomalacia (pronunciation: \in-ˌsef-ə-lō-mə-ˈlā-sh(ē-)ə\; ICD-9: 348.89) refers to cerebral softening or loss of brain tissue or parenchyma.
It is most commonly seen in the anterior frontal and temporal lobes. This is one of the most severe complications of brain injury (1,3)
In neonates and infants, there is what we call multicystic encephalomalacia. As the term implies, a number of cystic cavities or spaces are observed after the neonate or infant undergoes cerebral hypoxia and/or ischemia(4).
Encephalomalacia occurs with or without gliosis.
Gliosis is defined as multiplication of glial cells in the brain that may occur in response to a brain injury. This is observed under the microscope. In contrast with gliosis, encephalomalacia is a gross pathology of the brain(5)
Causes of Encephalomalacia
Encephalomalacia is primarily caused by disrupted blood flow into the brain leading to liquefactive necrosis and frank loss of brain parenchyma. The following are the most common causes of encephalomalacia(4,5):
- Cerebral ischemia
- Cerebral infarction
- Cerebral hemorrhage
- Traumatic brain injuries
- Cerebral infections: Encephalitis, meningitis
- Surgery
- Leptomeningeal cysts
For multicystic encephalomalacia in newborns and infants, the main culprit is brain hypoxia possibly due to the following (6,7):
- Asphyxia
- Twin-to-twin transfusion
- Encephalitis
- Meningitis
- TORCH: Toxoplasmosis, Rubella, Cytomegalovirus (CMV), Herpes simplex virus (HSV)
Pictures
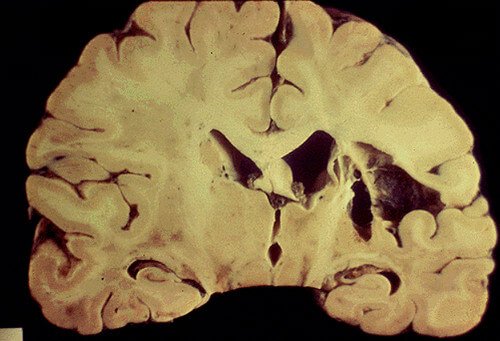
Picture 1: Gross cystic encephalomalacia caused by cerebral infarction. Also in this picture is the noticeable enlargement of the ipsilateral ventricle.
Image Source: http://spelunker.downstate.edu/ms/source/ms_render_media.asp?media_request=2527

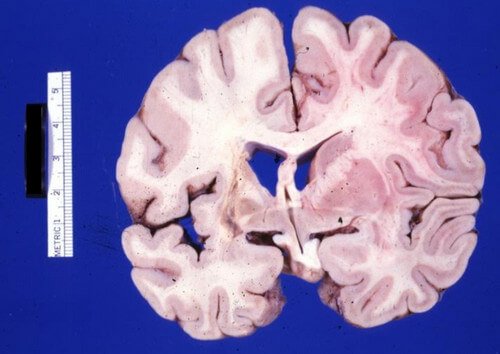
Picture 2: Gross cystic encephalomalacia of the frontal lobe caused by a recent cerebral hemorrhage.
Image Source: Pathology Education Informational Resource (PEIR) Digital Library. Available from: http://peir.path.uab.edu/library/picture.php?/3226
Picture 3: Gross cystic encephalomalacia in the left basal ganglia internal capsule with the case of dilated cardiomyopathy.
Image Source: Pathology Education Informational Resource (PEIR) Digital Library. Available from: http://peir.path.uab.edu/library/picture.php?/8616

Picture 4: Gross cystic encephalomalacia as a subcortical lesion in the Broca’s area.
Image Source: Pathology Education Informational Resource (PEIR) Digital Library. Available from: http://peir.path.uab.edu/library/picture.php?/9751

Picture 5: Encephalomalacia on axial noncontrast CT scan
Image Source: Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org, rID: 22285

Picture 6: Encephalomalacia after middle cerebral artery (MCA) infarction
Image Source: Case courtesy of Dr Roberto Schubert, Radiopaedia.org, rID: 15985

Picture 7: Encephalomalacia after MCA stroke seen on coronal noncontrast CT scan
Image Source: Case courtesy of Dr Bruno Di Muzio, Radiopaedia.org, rID: 19286
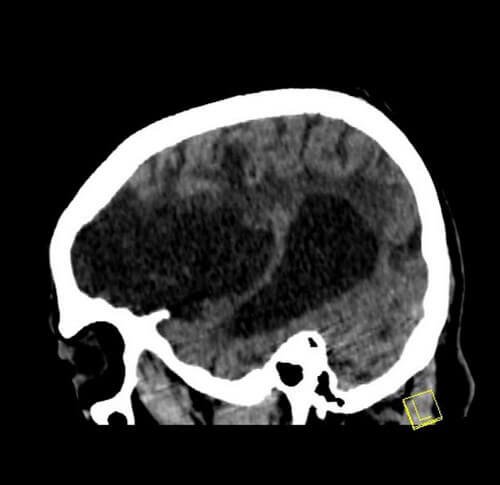
Picture 8: Encephalomalacia after MCA stroke seen on sagittal noncontrast CT scan
Image Source: Case courtesy of Dr Bruno Di Muzio, Radiopaedia.org, rID: 19286
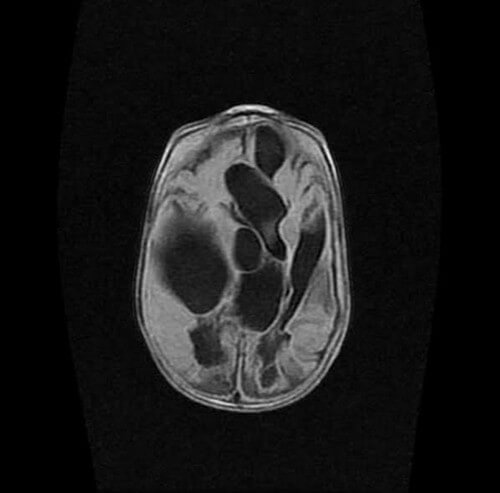
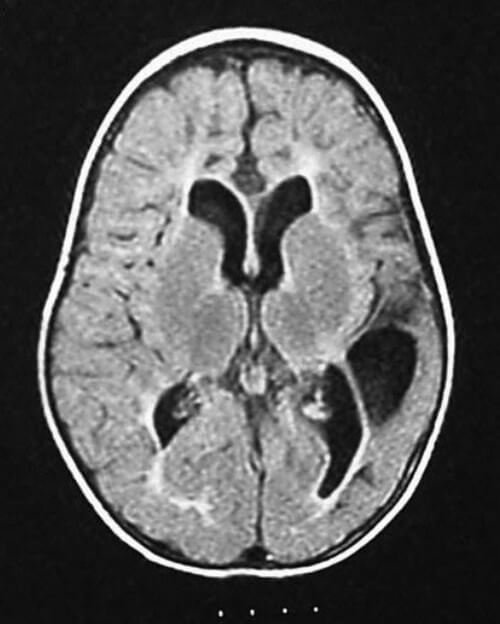
Picture 9: Multiple cystic encephalomalacia on MRI axial fluid attenuated inversion recovery (FLAIR)
Image Source: Case courtesy of Dr Arthur Daire, Radiopaedia.org, rID: 31349

Picture 10: Multiple cystic encephalomalacia on MRI coronal T2-weighted image
Image Source: Case courtesy of Dr Arthur Daire, Radiopaedia.org, rID: 31349
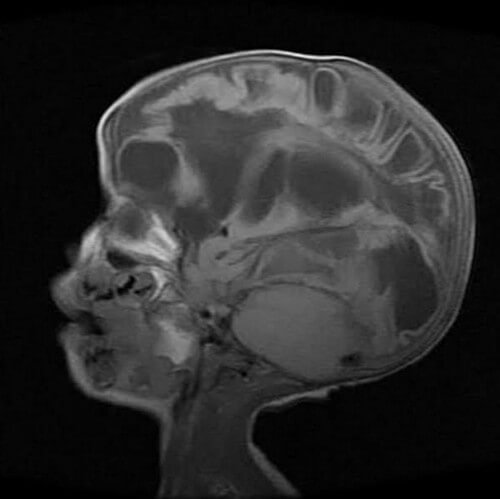
Picture 11: Multiple cystic encephalomalacia on MRI sagittal T1-weighted image
Image Source: Case courtesy of Dr Arthur Daire, Radiopaedia.org, rID: 31349
Picture 12: Cystic encephalomalacia is seen in the left temporal and parietal parts of the brain. The child (1 year and 4 months old), who had anoxia at birth, is suffering from cerebral palsy. Cystic encephalomalacia may be due to periventricular leukomalacia with infarction on the left cerebrum.
Image Source: Abdel-Hamid HZ. Cerebral Palsy. Medscape/Emedicine.
Diagnosis
Diagnosis of encephalomalacia can be done with the use of computed tomography (CT) scan or magnetic resonance imaging (MRI).
In encephalomalacia, there is depletion of a certain part of the brain parenchyma and decreased brain volume most frequently seen in the anterior frontal and temporal lobes. More often than not, encephalomalacia comes with gliosis (proliferation of glial cells) and Wallerian degeneration (degeneration of axons and myelin sheaths)(5).
It can also be performed during autopsy procedures wherein the pathologist grossly sees decreased consistency or disrupted margin of the brain tissue(4).
Focal post-traumatic brain injury like that in cerebral contusions and hematoma yields a localized form of encephalomalacia. Gliosis is a reaction of the brain when there is brain injury. In cases of traumatic brain injury, the area of encephalomalacia is surrounded by gliosis. CT scan reveals lucent (black) areas of the brain which correspond to the tissue loss, along with ventricular enlargement near the affected area.
On the other hand, MRI yields macrocystic encephalomalacia or obvious cavitations of the brain clearly seen on fluid attenuated inversion recovery (FLAIR) images. This is surrounded by more opaque T2 signal intensity which defines the microcystic changes and gliosis of the adjacent injured brain tissue(7).
All newborns and infants who had asphyxia, cerebral infection, or intracranial hemorrhage should undergo cranial sonography to rule out multicystic encephalomalacia. It is critical for this to be diagnosed as early as possible because as the disease progresses, the prognosis becomes so much worse than it already is(6).
Treatment and Prognosis of Encephalomalacia
As with other disease entities, you have to know the underlying condition to treat encephalomalacia but unfortunately, it will be very difficult because even the treatment has its consequences, like when a surgeon removes the severely damaged part of the brain, the surrounding brain tissue reacts by changing its consistency. Furthermore, treatment outcomes are not definite.
It cannot be accurately predicted. Even with appropriate treatment, we cannot exactly be sure what is going to happen to the patient. Encephalomalacia has no cure because neurons or brain cells do not regenerate once destroyed(3).
For multicystic encephalomalacia, prognosis is also very poor. It is not immediately observed among newborns because there are no signs and symptoms for this even if the disease is already there. It only becomes apparent during infancy period because parents or caregivers might notice the late motor developmental milestones of the child. Only then will multicystic encephalomalacia will be diagnosed, when there is already severe functional deficiency. Cystoperitoneal shunts or cyst taps are proven to be effective in managing multicystic encephalomalacia(6).
Complications
Encephalomalacia is an extremely serious brain condition and needs immediate attention of the neurologists. If left untreated, fatal sequelae might occur. The following may be the possible complications of encephalomalacia(2,3):
- Functional disability
- Seizures, especially in alcoholic patients
- Coma
- Death
References
- Merriam-Webster Medical Dictionary. Available from: http://www.merriam-webster.com/medical/encephalomalacia
- Ropper AH & Samuels MA. Adams & Victor’s Principles of Neurology, 9th edition. The McGraw-Hill Companies, Inc. 2009.
- Encephalomalacia Caused by Head Trauma. Passen Law Group. Available from: http://www.passenlaw.com/encephalomalacia-caused-by-head-trauma/
- Karaman E, et al. Encephalomalacia in the frontal lobe: complication of the endoscopic sinus surgery. J Craniofac Surg. 2011 Nov;22(6):2374-5. doi: 10.1097/SCS.0b013e318231e511.
- Knipe H, et al. Encephalomalacia. Radiopaedia. Available from: http://radiopaedia.org/articles/encephalomalacia
- Stannard MW & Jimenez JF. Sonographic Recognition of Multiple Cystic Encephalomalacia. AJNR 4:1111-1114, September/ October 1983 0195-6108/ 83/ 0405-11 11.
- Hodler J, Von Schulthess GK, Zollikofer C. Diseases of the Brain, Head & Neck, Spine 2012-2015: Diagnostic Imaging and Interventional Techniques. Springer Science & Business Media. 2 Sep 2012.