What is Torus Palatinus ?
Torus palatinus is a benign peculiarity wherein there is a bony outgrowth on the palate.
It is a normal bump on the roof of the mouth. It is one of the most common exostosis involving the oral cavity. It is not cancerous, nor it is painful or sore.
It comes in different shapes: nodular, spindle-like, lobular, or irregular. It is hard upon palpation and radiography shows opacity on this area due to the bone’s density. Since it is normal, there is no symptom associated with it.
Histologically, torus palatinus shows normal features of a typical bone. It is composed of outer cortical plate and inner cancellous zone [1, 2].
Torus Mandibularis
Torus mandibularis occurs on the lingual areas of the mandible that is near the cuspid and first bicuspid teeth. It can be unilateral or bilateral. The latter is more common occurring in 80% of cases [1, 3].
Torus Palatinus Causes
- Genetic and ethnic factors: Development of torus palatinus in parent/s poses a 40-64% chance that their offspring will have it too. If neither of the parents has it, there is a
- 5-8% chance that a child will have it.
- Bruxation and clenching
- Injury or trauma to bones of the oral cavity
- Forceful mastication can introduce stress to the bicuspids, eventually developing torus mandibularis [4, 5].
Prevalence
- Torus palatinus occurs in 20% of the general population. Torus mandibularis occurs in 6-40%.
- It mostly appears after puberty.
- It is generally seen among adults.
- For children in 5-15 age groups, there is 30.9% occurrence and it was shown that females are more likely to develop it.
- Torus palatinus is more common among females. Torus mandibularis is more common among males.
- Many Mongols, Asians, Eskimos, and Native Americans develop this bony exostosis [1, 4].
Treatment and Surgery
Torus palatinus does not need to be treated since its essential features appear to be normal. It is simply an anatomical variance that does not affect everyone of us.
Surgical removal offers a solution if torus palatinus causes a problem in the placement of dentures or dental prosthesis.
Under local or general anesthesia, the maxillofacial surgeon stains the torus palatinus to increase its visibility. He will incise on that area to expose the underlying tissue. The midpalatal suture expands and it applies force to the center of the bone. This results to removal of the torus palatinus.
Postoperative complications are minimal, including bleeding, swelling, and infection. The prognosis is very good. The patient fully recovers from the surgical wound after 3-4 weeks [6].
Torus Palatinus Photos

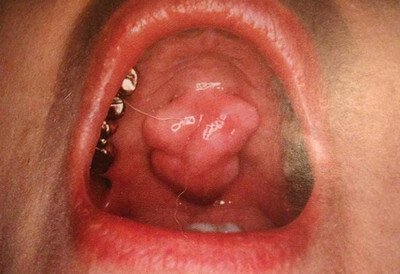
Picture 1: Torus Palatinus
Image Source: nejm.org

Picture 2: Palatal Tori
Image Source: nejm.org

Picture 3: Palatal Tori
Image Source: dentallecnotes.blogspot.com
Picture 4: Lobulated Torus Palatinus
Image Source: studyblue.com

Picture 5: Maxillary Torus Palatinus
Image Source: wikipedia.org

Picture 6: Torus Mandibularis
Image Source: nejm.org
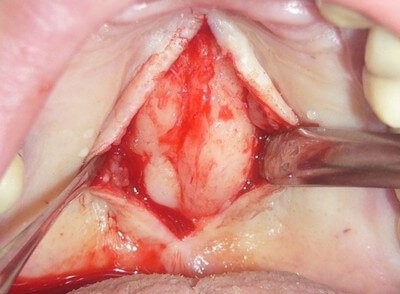
Picture 7: Torus Palatinus Explored
Image Source: pictures.doccheck.com

Picture 8: Radiograph of Torus Palatinus
Image Source: rad.usuhs.edu
References:
- Laskaris G, Color Atlas of Oral Diseases, Thieme 2003, p 11
- Eversole LR, Clinical Outline of Oral Pathology: Diagnosis and Treatment, PMPH-USA 2011, p 250
- Doherty GM & Way LW, Current Surgical Diagnosis & Treatment 12th
- DeLong L & Burkhart N, General and Oral Pathology for the Dental Hygienist, Lippincott Williams & Wilkins 2013, p 485
- Rajendran R, Shafer’s Textbook of Oral Pathology 6th edition, Elsevier India 2009, p 154
- Maxillary/Palatal Tori – Removal, Causes, and Treatment accessed on http://dentalmandibulartori.blogspot.com/2013/06/maxillarypalatal-tori-removal-causes.html edition, McGraw-Hill 2006
