What is the Vagus Nerve (CN X) ?
The Latin “vag” means “vagrant” or “wandering.” Knowing its distribution throughout the body, it is fit to call the vagus (pronunciation: VAY-gus) nerve as such [1, 2].
Unlike the other cranial nerves, vagus nerve is spread in different organs, making its functions much more appreciated.
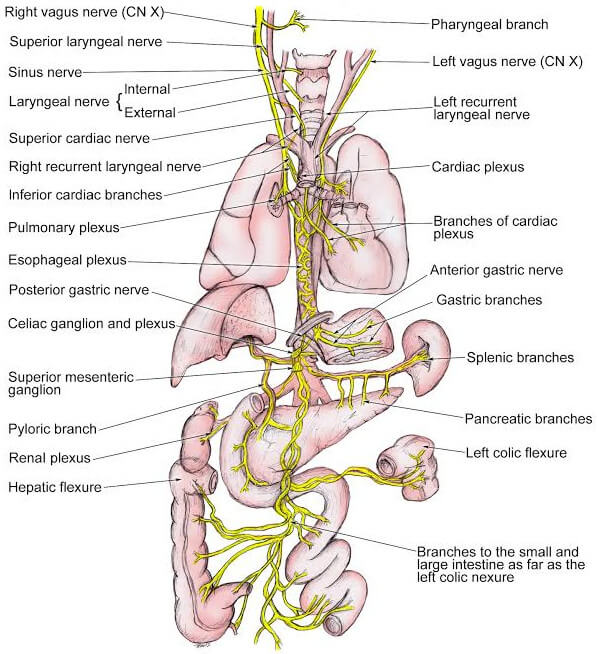
Vagus nerve is the tenth among the 12 cranial nerves. It stems out from the medulla oblongata and spreads out to the neck, chest, and abdomen. In the cervical area, it rides along with the common carotid artery and internal jugular vein.
Branches of the Vagus Nerve
Embryology
The vagus nerve innervates the outgrowths of the 4th branchial arch through the superior laryngeal nerve and of the 6th branchial arch through the recurrent laryngeal nerve. They form the anatomical structures of the pharynx and larynx [3].
On the left side, the 6th arch artery gives rise to the ductus arteriosus and the 6th arch nerve gives rise to recurrent laryngeal nerve. On the right side, the 6th arch artery normally disintegrates so the right recurrent laryngeal nerve associates itself on the right subclavian artery, which is the 4th arch artery [2].
Origin, Branches, and Pathway
Let us trace where the vagus nerve starts and ends.
- It all starts from the medulla.
- The rootlets go the the jugular foramen.
- Inside this hole are the jugular and nodose sensory ganglia.
- The one that passes through the lateral side of the skull is the auricular branch. It receives sensations from the ears.
- The vagus nerve becomes a part of the carotid sheath. Anterior to it are the common carotid artery and internal jugular vein.
- It gives off pharyngeal branch which is further divided into internal and external branches.
- On the base of the neck and upper portion of the thorax, cardiac and tracheal branches are appreciated. Stimulation of the cardiac branch causes bradycardia. The tracheal branch is a sensory branch.
- The recurrent laryngeal nerve is found in between the trachea and esophagus. It travels down to the mediastinum dividing into left and right parts. The left branch goes along with the ligamentum arteriosum and the right goes with the subclavian artery.
- The vagus nerve composes the esophageal plexus. It pierces the diaphragm and penetrates the abdominal viscera.
- The nerve fibers form the celiac, mesenteric, and myenteric plexuses.
- It advances to the lesser curvature of the stomach to give rise to hepatic branches and nerves of Latarjet. The latter innervates the pyloric antrum [2].
Photos of Anatomy: Where is the Vagus Nerve Located?
Sensory Neurons
Sensory axons of the vagus nerve come from the ears, pharynx, larynx, epiglottis, cervical muscles, carotid sinus, carotid and aortic bodies, and thoracic and abdominal viscera. They have cell bodies in the superior and inferior ganglia. The jugular foramen serves as a passageway for these sensory neurons and they terminate in the medulla and pons.
Motor Neurons
The branchial motor neurons of the vagus nerve come from the nucleus ambiguous of medulla oblongata and they innervate the muscles of the throat, particularly the soft palate, pharynx, larynx, and upper esophagus. These are responsible for swallowing, speaking, and coughing.
Below the neck up to the abdomen, the autonomic motor neurons of the vagus nerve perform their parasympathetic functions.
The efferents from the dorsal motor nucleus of the vagus go down and innervate the heart, lungs, and gastrointestinal tract. The smooth muscles contract to facilitate respiration and peristalsis. Vagus nerve stimulation also causes bradycardia [4, 5].

Picture 1: The Cranial Nerves
Image Source: alanatomy.com

Picture 2: The Origin and Distribution of the Vagus Nerve
Image Source: what-when-how.com

Picture 3: Parasympathetic Innervation
ImageSource: intranet.tdmu.edu.ua
 Picture 4: Vagus Nerve Pathway
Picture 4: Vagus Nerve Pathway
Image Source: helenpapas.wordpress.com
 Picture 5: Vagus Nerve and the Organs it Supplies.
Picture 5: Vagus Nerve and the Organs it Supplies.
Image Source: legacy.owensboro.kctcs.edu
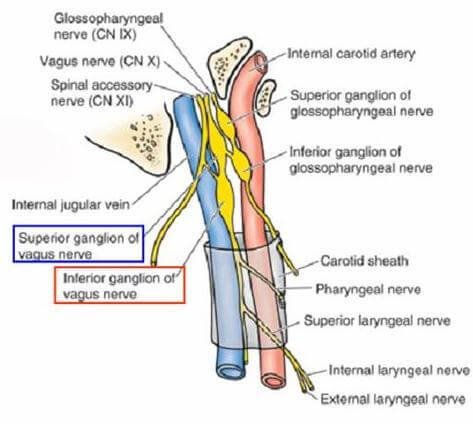 Picture 6: Superior and Inferior Ganglia and the Carotid Sheath
Picture 6: Superior and Inferior Ganglia and the Carotid Sheath
Image Source: studyblue.com
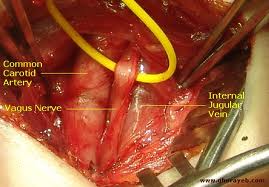 Picture 7: The vagus nerve is found in between and posterior to the common carotid artery and internal jugular vein.
Picture 7: The vagus nerve is found in between and posterior to the common carotid artery and internal jugular vein.
Image Source: ghorayeb.com

Picture 8: Nerve Supply of the Larynx
Image Source: embryology4genius.weebly.com
Function: What does the Vagus Nerve Do?
The vagus nerve has a mixed function: sensory and motor.
Sensory functions include
- Sense of taste
- Feeling of hunger
- Feeling of gastric fullness
- Abdominal pain and discomfort
Parasympathetic stimulation of the vagus nerve increases the muscle tone, strength, and peristalsis of the intestines thereby intensifying its motor actions [6].
Motor functions include
- Swallowing
- Speech function
* (These first two in the list are the main functions of the vagus nerve [2].) - Gastrointestinal movement
- Slow pumping of the heart
- Constriction of the bronchi [1]
Clinical (Neurologic) Test: How do you Stimulate It?
The integrity of the vagus nerve may be checked by stimulating the gag reflex or pharyngeal reflex. Do this by tapping the pharynx on its lateral side using a spatula or a tongue depressor. Normally, the muscles of the pharynx will contract and that will cause the patient to gag.
To test soft palate innervation, instruct the patient to say “ah.” The soft palate should rise up and the uvula should go backwards. If there is a lesion on the vagus nerve, the elevation of soft palate and uvula will be unequal and they diverge away from that damaged part [3].
If there is hoarseness or absence of voice, the recurrent laryngeal branch of the vagus nerve which controls the laryngeal muscles must be affected. Examine with the use of laryngoscope. It may show abductor paralysis [7].
Clinical Importance
Vagal Reflexes
As discussed, the vagus nerve has the most extensive distribution among the cranial nerves. This makes it possible for an organ to be vaguely associated with another organ which may not be categorized within the same body system.
For example, if there is a discomfort behind the external auditory meatus, the patient develops symptoms such as fainting, coughing, or vomiting. Fainting or syncope is caused by reflex bradycardia. Coughing happens become of the sensation perceived by the bronchial tree. Vomiting occurs when alimentary canal is stimulated.
Vagotomy
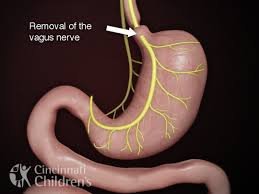
Picture 9: Site for Vagotomy
Image Source: cincinnatichildrensblog.org
Vagotomy is a procedure wherein a branch of the vagus nerve is cut. Usually, the nerves of Latarjet which supply the stomach are cut to treat gastric ulcer. Vagus nerve facilitates peristalsis of the gastrointestinal tract. Secretion of gastric acid is relevant in the process. If the vagus nerve in this area is cut, there will be less gastric acid secretion and decreased motility, thereby reducing the patient’s pain.
Thyroid Surgery
The superior laryngeal artery and inferior thyroid artery of the thyroid gland are proximal to the branches of the vagus nerve. The vagus nerve innervates the muscles that abduct the vocal cords. During thyroid surgery, proper identification of these structures is extremely important because when damage to the recurrent laryngeal nerve occurs, the vocal cords will be adducted. This will cause breathing problems.
Referred Pain
If a patient has hypopharyngeal tumor, there may be a referred pain from the pharynx and larynx to the ear.
Change in Voice
The vocal cords are controlled by the vagus nerve. There will be a change in the patient’s voice in the presence of a tumor in the left mediastinum. It causes the left recurrent laryngeal nerve to shift medially [2].
Damage to the Vagus Nerve : Disorders
Vagus nerve is very important. Damage to both nerves will put the patient in a critical condition. Depending on the extent of damage, the patient may be unable to taste his foods properly and he may even find it hard to swallow it (dysphagia). There will be hoarseness of voice and speech problems. Gastrointestinal motility will be impaired as well. If it is serious enough, it causes bronchodilation (widening of diameter of the bronchi) or tachycardia (fast heart rate) [1, 4].
References
- Saladin KS, Anatomy & Physiology: The Unity of Form and Function 5th edition, McGraw-Hill 2010, p 557
- Monkhouse S, Cranial Nerves Functional Anatomy, Cambridge University Press 2006, pp 86-91
- Hansen JT, Netter’s Clinical Anatomy 2nd edition, Saunders 2010, p 436
- Tortora GJ & Derrickson B, Principles of Anatomy and Physiology 13th edition, John Wiley & Sons Inc 2012, p 567
- Greenstein B & Greenstein A, Color Atlas of Neuroscience, Thieme 2000 p 228
- Lippincott Professional Guides, Anatomy & Physiology 2nd edition, Lippincott Williams & Wilkins 2002, p 131
- Snell RS, Clinical Anatomy by Systems, Lippincott Williams & Wilkins, p 229