Noticing an occult blood in stool can be very frightening. It can signal a serious problem and so it is important to have it checked right away. There are a lot of reasons for blood in stool. The amount of blood varies from one person to another.
Some people experience a bit of blood while others have a large amount of blood in the stool. A fresh blood in stool medical term is hematochezia. On the other hand, a dark stool or medically known as melena can suggest internal bleeding. (1, 2)
What are the associated symptoms?
There is mucus and blood in stool. Other associated symptoms include:
- Vomiting
- Abdominal pain
- Diarrhea
- Weakness
- Weight loss
- Difficulty of breathing
- Palpitations (2)
Picture of blood in stool
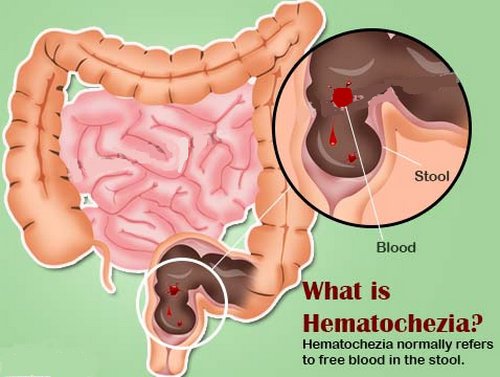
Image 1 : An image of the gastrointestinal tract outlining the possible location of blood
Photo Source : www.epainassist.com
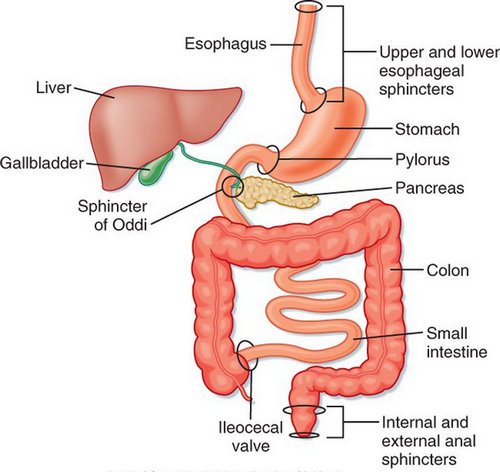
Picture 1 : An anatomical representation of the gastrointestinal tract
Photo Source : s-media-cache-ak0.pinimg.com
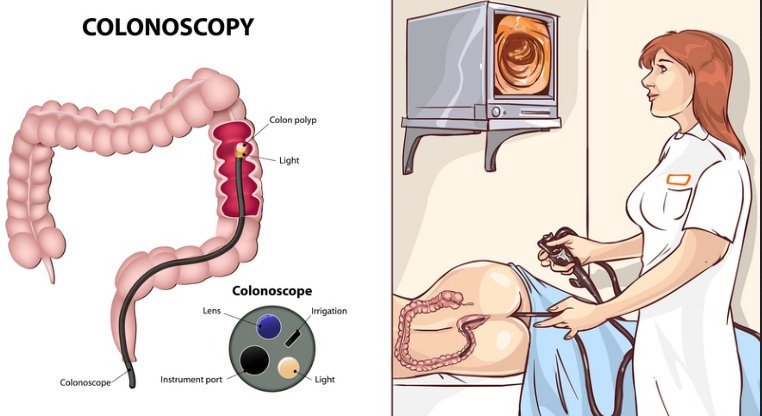
Image 3 : A picture that shows how colonoscopy is done
Picture Source : d2if36jingo4w0.cloudfront.net
What can cause blood in stool?
What does blood in your poop mean? Blood in the stool could suggest that something is wrong in your digestive tract. There could be a possibility of bleeding in the GI tract. Most of the time, the amount of blood is small that it can easily be detected on fecal occult test. If the bleeding is in large amount, then it could suggest a serious problem and warrants immediate medical attention. Possible reasons for blood in stool include the following:
- Piles/Hemorrhoids – the blood vessels in the rectal area are swollen. If your poo is hard, there is a possibility of bleeding. (2)
- Diverticular disease – Can you bleed with diverticulitis? Diverticula are tiny pouches projecting the colon wall. A bleeding is possible if the diverticula gets infected. (3)
- Anal fissure – It pertains to small cut or tear in the lining of the anus. It can be due to passage of a hard and large tool. It can be very painful and causes bleeding.
- Colitis – It is the inflammation of the colon. It can be caused by inflammatory bowel disease. If proper medication and management are not given, the patient could suffer from gastrointestinal bleeding, which leads to the presence of blood in the stool.
- Angiodysplasia – It is a condition characterized by sensitive and abnormal blood vessels. Even the simplest pressure could lead to bleeding.
- Peptic ulcer – It is an open sore, which can be present in various parts of the GI tract such as the duodenum, stomach, and upper end of the small intestine. Peptic ulcer is usually caused by H. pylori, but it could also be an adverse effect of medications such as ibuprofen, aspirin, and naproxen. (4)
- Polyps or cancer – A polyp is a benign growth that once gets out of control, could grow bigger and bleed. Over time, it can lead to cancer. Colorectal cancer causes bleeding, which is responsible for the presence of blood in the stool. Colorectal cancer is one of the most common cancers in America. (4, 5)
Diagnosis and Treatment
To come up with the best blood in stool treatment, it is important to properly diagnose the condition. The doctor will thoroughly evaluate the bleeding in the stool. The color of the blood has a lot to do with the root cause of the problem.
A black, tarry stool is an indicator that there is a problem in the upper part of the gastrointestinal tract. If the color of the blood is bright red or maroon, it is an indicator that something is wrong in the lower gastrointestinal tract. It could be due to diverticulitis or haemorrhoids. (5)
Various diagnostic procedures are used to detect the root cause of the problem. They include the following:
- Nasogastric lavage – This procedure tells exactly where the source of bleeding is. In this procedure, a tube is inserted into the stomach through the nose to remove the content of the stomach. If there is no blood in the upper GI tract, the source of bleeding could be in the lower GI tract. It could also be possible that the bleeding already subsided.
- EGD (Esophagogastroduodenoscopy) – An endoscope is inserted through the mouth going down the esophagus, stomach, and duodenum. This procedure is done to accurately detect the source of bleeding.
- Colonoscopy – It is somewhat similar to that of the EGD. The difference is that in colonoscopy, the scope is inserted through the rectum to have a clear view of the colon. It can also be used to collect a tissue sample for biopsy.
- Enteroscopy – This procedure is specifically for the small intestines. The patient should swallow a capsule with a tiny camera, which transmits images to video monitor as it passes through the gastrointestinal tract.
- Barium X-ray – It uses a barium, which is a contrast medium that makes the gastrointestinal tract visible on x-ray. The patient has the option to swallow the barium or have it inserted into the rectum.
- Radionuclide scanning – A small amount of radioactive material is injected into the vein. To see the images of blood flow in the GI tract, a special camera is used. This can help detect the source of bleeding.
- Angiography – A special dye is injected into the vein and its purpose is to make blood vessel visible on CT scan or X-ray.
- Laparotomy – This is an invasive medical procedure in which the doctor opens and examines the abdomen. This test should be the last resort. It can only be done if all other diagnostic procedures fail to detect the root cause of the bleeding. (5, 6, 7,8)
Note: A laboratory test in the form of blood stool is ordered to watch out for any signs of bacterial infection, anemia, and blood clotting problems.
Treatment and Management
The primary goal of treatment is stop immediately stop the bleeding. One of the common approach is to inject a substance to the bleeding site and treat it with an electric current/laser. Some doctors prefer to clip the bleeding vessels. The doctor can also inject a special type of medicine into the blood vessels to immediately stop or at least somehow control the bleeding. (9, 10)
The remedy does not end in stopping the bleeding. The root cause should be determined so as to avoid the problem from happening again. As with the treatment, it varies depending on the cause of the problem. If it is caused by bacteria, an antibiotic is prescribed. If it is caused by colitis, an anti-inflammatory medication should be given to the patient. A cream or suppository is required if the bleeding is caused by haemorrhoids. On the other hand, if the bleeding is caused by polyps, a surgery is warranted.
There are simple measures that you can do to stop, control, and prevent bleeding. A blood in the stool can be prevented from happening again if you eat foods rich in fiber. This is helpful, especially if you are constipated. Constipation can aggravate haemorrhoids, which increases the chance of bleeding. If you have blood in the stool secondary to fissures, you can relieve the pain and bleeding by sitting in a warm bath. (9, 10)
References:
- www.webmd.com
- www.medicinenet.com
- www.mayoclinic.org
- www.womenshealthmag.com
- www.livestrong.com
- www.thrombocyte.com
- www.healthline.com
- https://en.wikipedia.org
- www.doctorshealthpress.com
- Everyone’s Guide to Cancer Therapy: How Cancer Is Diagnosed, Treated, and Managed Day to Day By Andrew Ko