What is a Thecal Sac : Definition and Structure
The thecal sac is a covering of the spinal canal that is filled with cerebrospinal fluid (CSF).
It houses the spinal cord and nerve roots. It is made up of outer arachnoid membrane and inner dura.
It is wider in females. The length is approximately until S1 to S3 vertebral levels. It elongates and moves upwards upon spinal flexion or bending forward. On the other hand, it shortens and moves downwards upon spinal extension.
It is anchored to the spine by the coccygeal ligament in its lower end [1].
Thecal Sac Compression
Causes of Compression
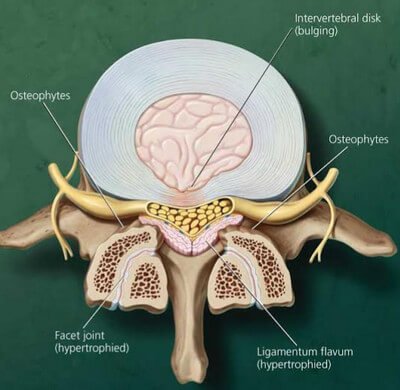
Picture 2: Herniated disc or enlarged ligamentum flavum substantially contributes to compression of the thecal sac.
Image Source: rheumatologynetwork.com
- Spinal neoplasms or tumors: The can cause spinal cord compression that impinges on the thecal sac and crowds the
- caudal nerve roots, resulting to cauda equina syndrome [2].
- Epidural lipomatosis: This refers to the abnormal build-up of epidural fat. Cushing’s syndrome and use of corticosteroids are the primary causes of epidural lipomatosis [3].
- Herniated discs
- Hypertrophied ligamentum flavum or facet joints
- Spinal canal stenosis
- Synovial cysts
- Osteophytes on the posterior bodies of the vertebrae
- Spondylolisthesis
- Spondylolysis
- Spinal fracture
- Spinal abscess and hematoma [4]
Thecal Sac Compression : Signs, Symptoms, and Diagnosis
- Lower back pain
- Muscle weakness
- Edematous nerve root
- Flattening of the thecal sac is noticed in patients with mild stenosis of the spinal canal.
- Thecal sac effacement is seen in patients with extradural lesions located in midline.
- Effacement of posterior epidural fat is observed in severe stenosis of the central canal.
- In spinal stenosis, the thecal sac is compressed by the protruding disc anteriorly and ligamentum flavum posteriorly, forming an hourglass shape.
- “Cloverleaf” or “trefoil” shape of the spinal canal for indentation of posterolateral thecal sac and severe central canal stenosis.
- If the cause is epidural lipomatosis, the characteristic “Y sign” or “stellate sign” is revealed on axial magnetic resonance imaging (MRI) because of the excess fat in the epidural compartment [3, 5, 6]
Treatment of Thecal Sac Compression
Before anything else, the patient must be given analgesics for the lower back pain. In order to treat thecal sac compression, identify the specific cause. Surgery is probably the best option because the primary problem in most cases is the structures that surround the thecal sac.
The surgeons will have to correct the anatomical structure itself in order to get rid of the impingement.
Other Conditions affecting the Thecal Sac
Ankylosing Spondylitis
The chief complaint for ankylosing spondylitis is chronic pain on the lower back that radiates to the groin and posterior thigh. X-ray shows a characteristic “bamboo spine” because of the damaged sacroiliac joints and bridging of the vertebrae.
Another hallmark for ankylosing spondylitis is the exaggerated expansion of the thecal sac in the lumbar area [7].
Chronic Adhesive Arachnoiditis

Picture 3: “Fanning” in the thecal sac is normal.
Image Source: radsource.us
Chronic adhesive arachnoiditis is an inflammation of the nerves and meninges of the spinal canal. It starts as an exudative reaction. As it progresses, fibrin accumulates forming strands of collagen that cause adhesion of the nerve roots towards the lining of the thecal sac.
Possible causes of adhesive arachnoiditis include trauma, meningitis, hemorrhage, myelography, surgery, radiation treatment, neurotoxic substances, or incorrect intrathecal administration of methylprednisolone acetate.
Fanning of the nerve roots over the lumbar area should be seen in the radiographic sagittal view of the thecal sac. However, they become absent when the nerves roots adhere with each other as seen in the pictures below [8, 9, 10].

Picture 4: There is no fanning of the nerve roots in the presence of arachnoiditis.
Image Source: radsource.us

Picture 5: Axial View of Empty Sac Sign in Arachnoiditis
Image Source: radsource.us
References:
- Postacchini F, Lumbar Disc Herniation, Springer Science & Business Media 1999
- Abrahm JL, Assessment and Treatment of PatientsWith Malignant Spinal Cord Compression accessed on http://www.oncologypractice.com/jso/journal/articles/0205377.pdf
- Fatterpekar G et al, The Teaching Files: Brain and Spine, Elsevier Health Sciences 2011
- Burgener FA & Herzog C, Differential Diagnosis in Computed Tomography, Thieme 2009
- Hasselink JR, Degenerative Spine Disease accessed on http://spinwarp.ucsd.edu/neuroweb/Text/sp-700.htm
- Tuthill H & Clifford PD, Lumbar Spine Stenosis accessed on http://www.amjorthopedics.com/fileadmin/qhi_archive/ArticlePDF/AJO/037080423.pdf
- Ropper AH & Samuels MA, Adams & Victor’s Principles of Neurology 9th Edition, McGraw-Hill Companies Inc. 2009
- Poe LB, Arachnoiditis is MRI Web Clinic, July 2007 accessed on http://www.radsource.us/clinic/0707
- Burgener FA & Meyers SP, Differential Diagnosis in Magnetic Resonance Imaging, Thieme 2011
- Skalski M & Millner T, Empty Thecal Sac Sign accessed on http://radiopaedia.org/articles/empty-thecal-sac-sign
